We met Sangita (name changed) at the crowded sub-district hospital in Jawhar in Maharashtra, which routinely sees about 200 out-patients every day. Her baby had been sick for a few days, and had developed skin rashes which worsened after a home-made ointment was administered by a local quack. Terrified of her child’s condition, she had to rush to the nearest hospital, about 20 km from her village.
But distance was not the only hurdle in getting basic healthcare for her child. After waiting for nearly two hours, she met the doctor who told her the child had a minor heat rash. While she felt relieved that her child’s condition was not serious, she was worried about the amount of money and time they had to spend to see a doctor. Her husband had lost a day’s wage, and they had spent almost Rs 100 to travel to the hospital.
Stories like Sangita’s are widely quoted and talked about as one of the key challenges in delivering primary healthcare to the remote populations in developing regions. In these regions, people living in the last-mile areas lack the most basic facilities required for human development and growth. Their villages are not connected by roads; they do not have access to reliable water or electricity supplies; mobile towers have not yet reached their villages; and access to primary healthcare, a fundamental right of every citizen, is severely missing in their lives, forcing families like Sangita’s to travel a long distance for medical treatment. These are villages of a few hundred or thousand people, which are too small for economies of scale to benefit them, and unfortunately, current programmes are heavily focused on higher levels of care.
Fixing the broken continuum of care
India has made reasonable progress in improving access to last-mile healthcare over the last decade. However, the improved access has not reached the 29 states equally. In addition, existing facilities, both public and private, face acute shortage of qualified personnel (fully trained doctors, lab technicians) as well as facilities and medical supplies.

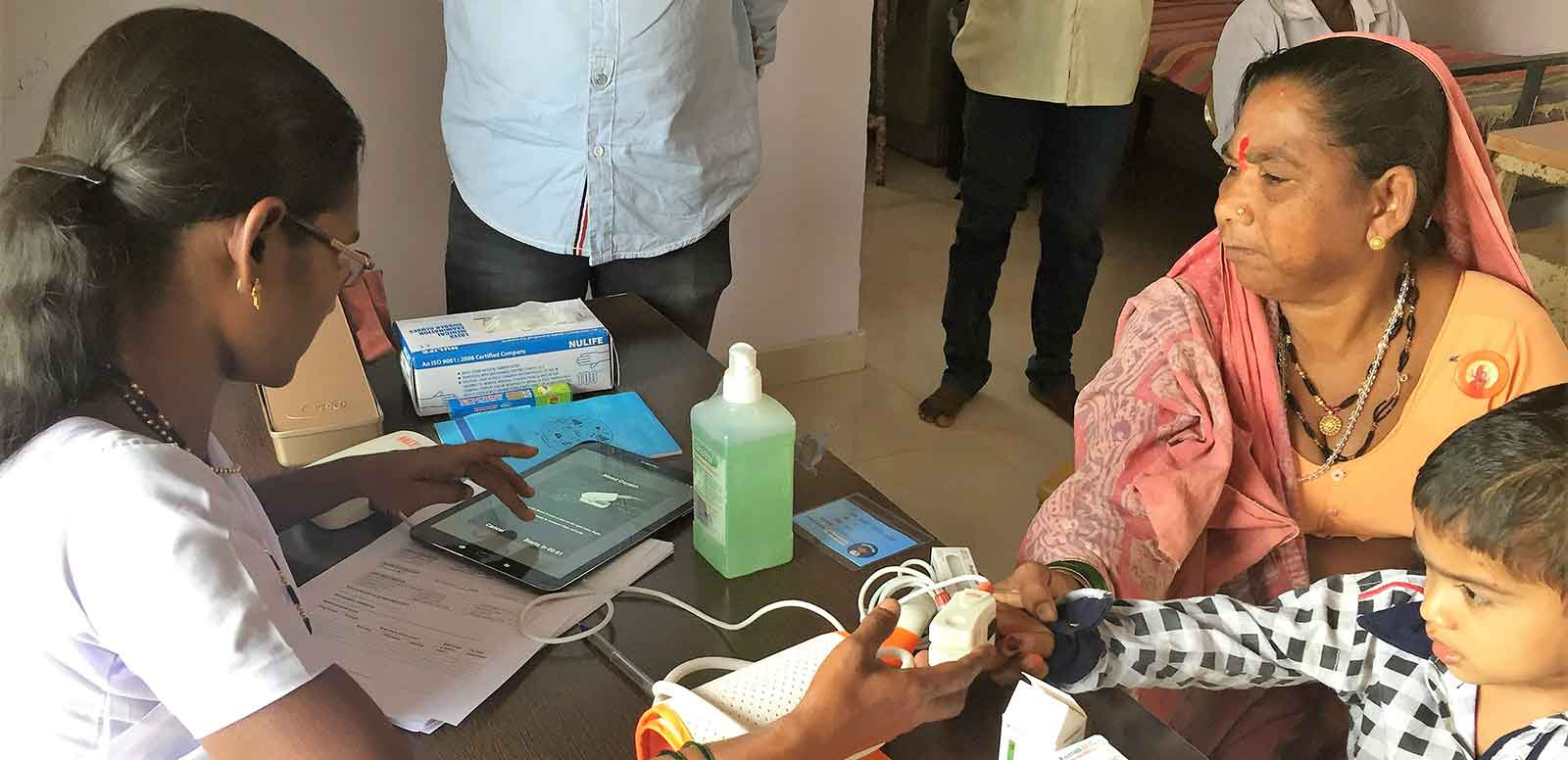
An ANM treats patients at a Bokarhatti clinic in Palghar district.
On the other side, auxiliary nurse midwives (ANMs) who are posted at sub-centres are clinically trained and qualified to treat ‘minor ailments’ and provide first aid. However, they remain grossly under-utilised, with their majority of their time dedicated to field-based data collection. The sub-centres are mostly non-operational due to the lack of facilities and clarity on services to be provided. In many cases, they end up being used to store medicines, or serve as living quarters for the ANMs.
What Sangita and her baby really needed was a primary healthcare clinic within a walking distance from their house. In the Indian healthcare system, these clinics are called sub-centres, typically catering to a population of about 5,000 people and with up to two ANMs and support staff. The ANM, when aided with simple, easy to use POC diagnostic tools, therapeutic devices and a simple mobile-based software to track patient data, can be effective tool to improve care delivery at the last mile.
Learnings from the field
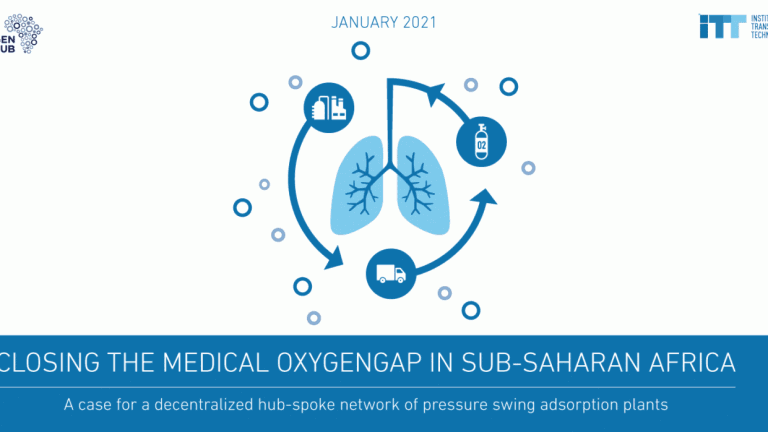
Trying out one such integrated approach, the Institute for Transformative Technologies (ITT) is working with the Zila Parishad in Palghar district of Maharashtra, and regional partners. The approach combines technology, improved clinical protocols, and patient engagement at the last mile, and over the last few months been deployed in two sub-centres of Palghar.

ANM treating patients at Pavarpada clinic in Palghar district.
At the centre of this model are the sub-centres, which function as spoke clinics, where the ANM is empowered with the best-in-class technology (a software platform to track patient data and point-of-care diagnostics), and standardised clinical protocols. PHCs, that are staffed with medical officers, serve as the hub for the sub-centres. The current pilot programme has been running in Jawhar block, Palghar district, with more than 300 consultations and 90% patient satisfaction rate recorded to date. There has also been a noticeable improvement (greater than 40% improvement in pre- and post-training test scores) in the ANM’s clinical skills, such as providing out-patient care for minor ailments, such as fevers, infections, ante-natal care etc.
As ITT continues to expand work across Palghar, we have identified a few key lessons. First, technology is a great enabler in changing people’s lives, but for it to be effective and result oriented, it needs the right delivery model with operational blueprints, training and clinical protocols. Second, for technology to be deployed for human development, an iterative, data-driven and user-centric approach is required. In our work, we have conducted multiple cycles of user-testing and research activities which help us identify challenges that rural healthcare providers and patients truly face. Without this, technology will be seen as the “enemy” that hinders them and adds to their burden.
The National Health Policy (2017) calls for upgradation for all 150,000 sub-centres in the country as ‘Health and Wellness Centres’ to provide improved primary care, with basic preventive, diagnostic, curative and referral facilities. As the required policies come through, it is time we define the right models to empower nurses and paramedics to deliver more at the last mile.
Krisha Mathur and her team are trying to create a financially sustainable healthcare model for the last mile in rural India. She is a senior manager at Institute for Transformative Technologies.